Instrumental Swallow Study Options?
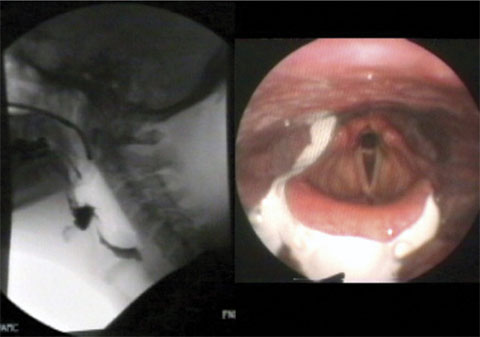
A Modified Barium Swallow Study (MBSS), also known as a videoswallow (VFSS), is used to instrumentally asses swallow function. It is completed in a radiology suite. This examination involves a radiologist, a radiology technician, a speech language pathologist (SLP), fluoroscopic xray equipment, and barium contrast. The patient is given a few consistencies of food and liquid mixed with barium (which appears on x-ray) to eat and drink. The patient must be sitting fully upright to not impede the xray view. The SLP is then able to assess the swallow while the fluoroscopy is turned on. This evaluation is completed fairly quickly during a handful of swallows in order to reduce radiation exposure for the patient.
The FEES (Fiberoptic Endoscopic Evaluation of Swallowing) procedure has revolutionized the field of dysphagia diagnostics and management, and is now being used more often than videofluoroscopic studies in many states across the nation because of many benefits listed below.
How does MOBILE FEES differ from a MBSS (videoswallow)?
- Takes place in the comfort of the patient’s living environment, eliminating the cost/need for transportation or patient chaperon
- Performed with the patient seated in his/her ‘natural’ eating position, as opposed to a videoswallow chair upright as possible
- Captures the “true picture” of what is happening at meals by the patient self feeding over time (assess for impulsivity, fatigue, postural variations, etc.)
- Uses ‘real food’ versus barium…which may alter the consistency of food/drink, may cause an increase in swallow dwell times, makes dry regular solids difficult to view, is known to cause constipation, and can be harmful to the lungs
- We supply an array of consistencies of food/liquid for the exam, but feel free to include ‘special request’ items or save the patient’s real medications to test
- Colored recordings allow for assessment of secretion management and tissue health compared to a black and white x-ray
- Provides distinct picture of anatomically why and where pills are “getting stuck” through direct visualization of anatomy
- Continuous recording of the entire study captures penetration/aspiration after the swallow and in between swallows (including esophageal backflow), which may be missed due to radiation time limits or when fluoroscopy is turned off
- No radiation exposure is beneficial to the patient and allows many observers in the room, which can increase dysphagia awareness among family and/or staff
- Because there is no radiation, the recording of FEES can last much longer enabling assessment for: fatigue, the effectiveness of swallow strategies in depth, reflux, and testing more challenging and difficult items
- ‘Bird’s eye’ superior view in color allows for evaluation of anatomy, unilateral weakness, vocal fold function, supraglottic airway closure, and secretion management (all important components for protection and prevention of aspiration)
- Can be performed on medically complex patients who may not tolerate transportation, obese patients who may not fit into a videoswallow chair, ventilator patients who may not be able to transport easily, patients who are in isolation and cannot leave a room, patients who are confused (dementia) who may not follow commands in an unfamiliar environment, patients with pressure ulcers or who are bed bound, and many more
- It is unlikely the primary SLP will be able to accompany the patient to the hospital, making it difficult for the hospital SLP to understand the full picture (i.e. patient eccentricities, normal eating pattern, pt’s potential to learn a specific strategy, specific items causing more trouble, etc.)
- The primary SLP can be present to provide valuable input and may bill for dysphagia treatment that same day (two minds at work is better than one outside mind who is unfamiliar with the patient)
- Procedure takes approximately 15-30 minutes to complete, significantly decreasing the hours the patient is at a hospital (no “lost” therapy minutes by PT/OT; no denial of ST claims the day of)
- NO need to schedule with hospital radiology, coordinate with hospital speech pathology, wait weeks for the appointment, set up transportation, arrange for patient chaperone, contact hospital SLP with specific information, or wait for the report back
- Quick turn-around time as we guarantee completion of procedure within 4 business days from your request
- Full report (including color photos) provided to you BEFORE we leave
- Digital recording of procedures are securely stored for future comparison of studies
- And remember, determining the etiology of the dysphagia will help lower the cost of caring for patients with swallowing problems, decrease re-hospitalizations, streamline treatment planning, improve therapeutic outcome statistics, aid in patient/family decision making, and increase patients’ quality of life/satisfaction!
